Background
Biliary Pseudolithiasis caused by Ceftriaxone is a rare condition characterized by jaundice with abdominal pain due to cholecystitis or acute pancreatitis. Usually seen in patients who were treated with ceftriaxone recently. Symptoms at presentation depend on the severity of the case and the blockage site of the biliary sludge. The treatment is supportive (most cases resolve spontaneously after withdrawal of Ceftriaxone) and The mean duration to resolution of biliary pseudolithiasis is about 15 days.
Case presentation
We herein report a rare presentation of ceftriaxone Pseudolithiasis in an 11-month infant with a mild hematologic disorder which was diagnosed after additional history from her mom. The patient underwent ERCP with three biliary stones removed and A stent was installed due to the stenosis of the Oddi. She was followed up for a year without any other biliary stones or blood transfusions. even when the strict protocol is followed clinicians must be alert to the potential of Forgetting some points of the medical family history and additional history should be taken when we suspected a Genetic disease.
Conclusions
The objective of this clinical case report is to highlight these unusual biliary stones after admitting ceftriaxone and focus on patient follow-up to avoid serious complications.
Background
Hereditary spherocytosis (HS) is the most common cause of hemolytic anemia as a result of an abnormal red cell membrane, in which these cells are round like a sphere. Spherocytes are red blood cells more fragile than the disk-shaped ones.
Early symptoms are jaundice, anemia, splenomegaly, and fatigue.
Most cases can be detected soon after birth. However, in some cases, the disease may still unnoticed until the child is four or five years old. Pigmented gallstones may bedeveloped as a complication of HS, where the detritus of the broken-down blood cells, unconjugated or indirect bilirubin, accumulating within the gallbladder.
Ceftriaxone is a new third-generation cephalosporin that has high activity against many gram-negative germs and reasonable activity against most gram-positive germs. Clinical studies have shown its efficacy and safety in patients with bacterial meningitis and respiratory tract infectious diseases. Because of its efficacy, safety, and convenient dosing schedule, ceftriaxone may become the preferred third-generation cephalosporin for the treatment of a lot of serious infections. (1) Ceftriaxone is excreted from the body by urine and bile. And its Side effects include diarrhea, rash and itching in adults and children. In laboratory test results, transient eosinophilia and elevated liver and kidney function tests occurred.
It also can lead to the formation of gallstones. Most patients are asymptomatic because the stone disappears immediately after stopping ceftriaxone,
making this condition called ceftriaxone-associated pseudolithiasis (2).
Ceftriaxone-associated pseudolithiasis was first described in 1988 by Schaad et al.
Because ceftriaxone, like bilirubin, can precipitate with calcium, ceftriaxone-associated biliary sludge is thought to be composed mainly of calcium-ceftriaxone complexes. Afterward, the precipitated sludge forms stones and may finally develop into ceftriaxone-induced biliary pseudolithiasis. (3, 4)
Case Presentation:
An 11-month premature Syrian female infant presented to the office by her mom complaining of high fever and lethargy. On scrutiny of her previous records, she was born at 28 weeks via cesarean section and admitted to the NICU for five days due to premature birth and respiratory disorders. She received all her vaccinations and complained of three episodes of respiratory infection treated with ceftriaxone she did not have any medical disorder after that.
The physical examination on admission revealed a pale appearance and lethargy with a high fever. Meningitis signs were negative. Her abdomen was flat and non-tender and had no rebound tenderness. No mass was palpated and Murphy’s sign was negative.
According to these symptoms she was diagnosed with nonfocal septicemia. Then, she was admitted to the hospital initiating the therapy with ceftriaxone 100mg\kg for five days.
While checking the infant on the fifth day looking for the foci of the inflammation, we noticed a dilation in the biliary tree on abdominal ultrasound, which was not present when the patient was admitted to the hospital.
Hematologic and other tests were ordered. The result is below:
hemoglobin 11 [normal range 9.5-14] g/L , platelet 231×103 [normal range 150 × 103 to 450 × 103] mcL , Liver function tests showed aspartate aminotransferase [AST] 35 [normal range 20–65] U/L and alanine aminotransferase [ALT] 32 [normal range 10–40] U/L) and gamma-glutamyl transferase (GGT) of 45 (normal range 15–110) U/L.
PT PTT, lipase, and electrodes all were normal.
After that we ordered MRI and the diagnosis of biliary stones was conferred. Figure (1,2).
At this time her mom said that the patient’s uncle
a blood disorder with multiple blood transfusions, according to that we requested a blood smear and what was shocking is that the patient has hereditary spherocytosis. Figure (3).
Under general anesthesia, the infant successfully underwent ERCP with three biliary stones removed and a stent was installed due to the stenosis of the Oddi sphincter.
The stent was removed after six months, and the patient was followed up via abdominal ultrasound for a year without any other biliary stones or blood transfusions.
We know that hereditary spherocytosis can present with anemia and hemolysis but the main point here is that ceftriaxone increases the rate of hemolysis, especially the biliary dilation noticed after five days of administrating ceftriaxone in an infant who had no previous jaundice nor blood transfusion even after one year of the stones ablation.
Discussion and Conclusions
Gallstones were considered to be infrequent in children and infants, but wide-spread use of ultrasonography has increased the diagnosis of cholelithiasis in the pediatric age.[6] The prevalence rate of gallstones in unselected pediatric populations ranges between 0.1-1.0% (7). Up to 75% of gallstones in children are pigment stones (8).
The causes of gallstones in children differs somewhat from in adults. They include hemolytic diseases, prematurity, total parenteral nutrition, ileal disease, congenital biliary diseases, some drugs and antibiotics (such as ceftriaxone) and there are cases remain idiopathic (6).
Cholelithiasis in the first year of life is associated with malformations and drugs (9).
Gallstones in children can manifest with typical biliary symptoms in almost half of cases, nonspecific symptoms in quarter of cases, asymptomatic in 20%,
or complicated in 5% (6). Children who presents with symptomatic gallstones are prone to complications. The complications include acute cholecystitis, pancreatitis and choledocholithiasis. (7).
Inflammation and fibrosis from the chronic passage of gallstones may lead to narrowing of the distal end of the bile duct and the proximal end of the pancreatic duct. Episodes of acute pancreatitis , chronic pancreatitis may be complications of stenosis of the oddi’s sphincter. The pain can be
relieved by transduodenal sphincteroplasty and transampullary septectomy(10). ERCP is safe and has a high success rate in children if it is performed by experienced specialists (11).
Hereditary spherocytosis is one of congenital hemolytic diseases. It is inherited as an autosomal dominant trait in 70% of cases. It is due to various mutations of genes that encode membrane proteins of red blood cells resulting in the formation of spherocytes(12). Spherocytes lack the flexibility and become fragile so that they rupture in the circulation. (12, 13). The clinical manifestations depend on the severity of hemolysis and range from asymptomatic patients with incidental diagnosis to severe forms which requires blood transfusions in early childhood(12). Anemia, jaundice, splenomegaly are all clinical presentations of hereditary spherocytosis. And because it is a hereditary disease, the family history may suggest the diagnosis. The risk of pigment gallstones formation increases in hereditary spherocytosis because of chronic hemolysis and patients should undergo cholecystectomy (12, 13). The probability of gallstones formation in HS is related to the patient age and is uncommon in children younger than 10 years (13).
Depending on the facts we presented above and whereas the patient is an infant, there is no prior history of anemia or jaundice, and the following of the patient did not reveal any problems, so we can decide that ceftriaxone accelerates the stones formation, especially after we have known that hereditary spherocytosis could be asymptomatic in some cases.
HS should be suspected in children presenting with one of the classic triads: hyperbilirubinemia splenomegaly, and anemia.
HS in children may also present with asymptomatic cholelithiasis of undetermined etiology.
In neonates, Jaundice is the most common finding of HS. Thus, neonates with hyperbilirubinemia of, unknown cause should be suspected complaining of HS particularly if they have a positive family historywe conclude that the presence of hereditary spherocytosis does not mean necessarily that it is the main cause of gallstones, especially in infants. We need to take the other causes into considerationbefore we do procedures unrequested like cholecystectomy.
Abbreviations
CTRX: ceftriaxone.
NICU: Neonatal intensive care unit.
ERCP: Endoscopic Retrograde Cholangio Pancreatography.
The Availability of data: Not applicable.
Ethics approval and consent to participate:
Not applicable.
Consent for publication
Written informed consent was obtained from the parents of the child for publication of this case report and any accompanying images and videos. A copy of the written consent is available for review by the editor of this journal.
Authors’ contributions
MA is the first author equally with MH, contributed to drafting, editing, reviewing, data collecting and bibliography.
MH is the first author equally with MA, contributed to drafting, editing, reviewing, data collecting and bibliography.
NM contributed to editing, reviewing, data collecting and bibliography.
JM is the mentor, contributed to supervising and reviewing.
All author reviewed and accepted the paper.
Acknowledgements
We wish to show our appreciation to Stemosis for Scientific Research, a Syrian Scientific Research youth association for the scientific environment they provide. We also wish to show our appreciation to DR. Hazem Kamil, a PR member at Stemosis for Scientific Research, for his technical support.
I, Nafiza Martini, as Stemosis for Scientific Research’s manager, express my sincere thanks and gratitude to Dr. Jaber Mahmoud for his cooperation with our administration of Stemosis for Scientific Research in many research papers and his moral support.
References

Figure 1.MRI imaging showing dilation in the biliary tree.

Figure 2. MRI imaging showing dilation in the biliary tree.
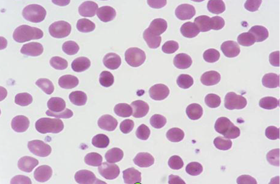
Figure 3. A spherocytosis appears in the patient’s blood smear